Objective
To generate health economical analyses of solutions in precision medicine as a basis for informed decisions with regard to the implementation of such solutions.
Activities
- Cost-utility analysis of CYP2C19: CYP2C19*2 Genotype- Guided Antiplatelet Therapy for Acute Coronary Syndromes after Percutaneous Coronary Intervention in Norway: A Cost-Utility Analysis. This is a master thesis by Mónica Gómez (UiO) that will be published on bigmed.no. The treatment described in the thesis is not common practice in Norway and it was recently referred to in Dagens Medisin.
- Cost-effectiveness analysis of genetic sequencing: this article will investigate genetic sequencing in patients with advanced cancer. It is a part of a larger project, or an extension to the professional collaboration, between Eline Aas and the research group MetAction. The group has accumulated significant amounts of data from follow-ups of patients who have undergone gene sequencing and are now equipped with a large number of longitudinal patient- and cost data. Next article will be published in the fall of 2020 and will be made available on bigmed.no.
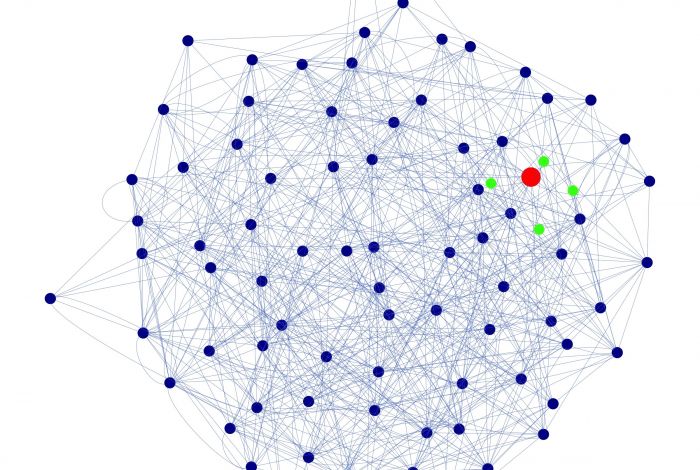
- AI / ML on treatment pathways: artificial intelligence, and more specifically, machine learning applied to pathways for patients with colorectal cancer (netDx). Involved: Eline Aas, Andrew H. Reiner, Arnoldo Frigessi and Vegar J. Dagenborg.
- Seminar: Precision Medicine: A Health Economic Perspective. Read more and access the recording via this link.
Deliverables
- Data from treatment pathways. To present arguments on the importance of getting access to detailed data of good quality from treatment pathways. These data are crucial to health economical evaluations. Barriers are listed as (not exhaustive): the legislation, consent, and the types of data that we can access systematically.
- Systems and routines. To describe the system, or routines, for the approval and financing of medical drugs and treatments related to precision medicine.
- System processes. To identify processes within the current system. For example, how approvals are evaluated with regard to the market access of medical drugs, as well as how patient treatments and medical drugs should be funded. These processes are taking place within the Norwegian Medicines Agency (NMA) and in decision making forums (for new methods). The basis for decision making can be found in guidelines issued by: the NMA, Norwegian Directorate of Health (NDH), in the Official Norwegian Reports (NOUs), as well as in the regulations.
- Precision medicine. To describe precision medicine in light of the current system. Unfortunately, the current system is not organized to manage precision medicine. Diagnostics and treatments are evaluated at separate levels and we need to figure out how to deal with uncertainty in research as few observations (n=1) also equal less comparators. Present how new medical drugs are financed (reimbursed) and solutions to how we can manage agreements between private and public actors.